HOSPITAL INFORMATION
The Centre is assigned with the tasks of realising early hospitalisation, specialised treatment, and early social comeback of patients suffering from spinal issues or spinal cord diseases caused by work, traffic, or accidents. To this end, it has secured expert specialised staff and state-of-the-art medical apparatus to maintain a high level of medical treatment, with the introduction of a new system and a concern for facilities and equipment from an entirely new perspective.
Moreover, the medical technology research department (Department of Assistive Technology and Design) was jointly established by the hospital to support the severely handicapped from the standpoint of rehabilitation technology. The research and rehabilitation staff are dedicated to the earliest possible comeback of the handicapped in close association with treatment and medical rehabilitation oriented to functional recovery.

Since 1979, we have treated patients with traumatic spinal cord injury from the acute phase to social return. Early surgery and high-quality rehabilitation have been offered. We treat patients with traumatic spinal injuries and most spinal diseases that require surgical treatment, such as degenerative disease, spinal deformity (adult or adolescent deformity), spinal tumour, spinal infection, etc. Our Spinal Injures Centre is one of the most well known hospitals for patients with spinal diseases, and one of the two largest spinal injury centres in Japan.
Medical Treatment Department
The Department of Orthopedic Surgery, Rehabilitation Medicine, and Urology are the key departments of the Medical Treatment Department. The co-operation of medical staff, including medical doctors, nurses, therapists, radiological technicians, laboratory technicians, medical engineering researchers, and medical social workers, plays a key role in team rehabilitation for the earliest possible social comeback of patients. To cope with injuries and diseases, it is crucial to provide proper treatment as early as possible to minimise injury and ensure smooth rehabilitation. Early and accurate operations for acute patients significantly affect treatment outcomes. In addition, accurate examination and treatments based on the current evidence for patients with urination disorders (e.g., neurogenic bladder and urinary tract infection), especially due to spinal cord injury, have been performed in the urology department.
In addition to the introduction of advanced special medication rendered with state-of-the-art medical apparatus and equipment, efforts are also concentrated on medical research toward further improvement of medical techniques in the specialised fields.

Rehabilitation Department
To improve fundamental physical ability, specialised staff members provide proper guidance and support from hospitalisation until the release of a patient by means of physical therapy, occupational therapy, activities of daily living (ADL) training, etc. An ample variety of treatments, training, appraisal apparatus, and equipment are installed, including a walk-assist robot, therapeutic electrical stimulations, and a gymnasium. Diversified expertise in spinal injuries and spinal cord diseases is utilised for bedside training soon after an operation, for bathing and excretory training based on preliminary home visitation and consultation, guidance of transferring to a car, proper wheelchair handling and wheelchair life guidance, and the manufacture of outfits and self-helping tools.



Nursing Department
Warm-hearted nursing to give patients a sense of contentment and relaxation along with enough communication is of the highest priorities. Nursing required for a specialised hospital is performed comprehensively: for example, care for the respiration of functional disorders, prevention of bedsores, excretory control, and maintenance of good posture in bed. Many considerations have been given to equipment, such as wide corridors enabling patients to move in bed and lift-type bathing devices in addition to spacious sickrooms and toilets adapted for wheelchair use, rails, and slopes fitted everywhere, and a comfortable courtyard.



What is special?
We have consistently treated severely paralysed patients from the acute to chronic phase because most patients are allowed to remain hospitalised the Centre until they are able to become independent (e.g., 6 months for paraplegic individuals and 1 year for tetraplegic individuals).
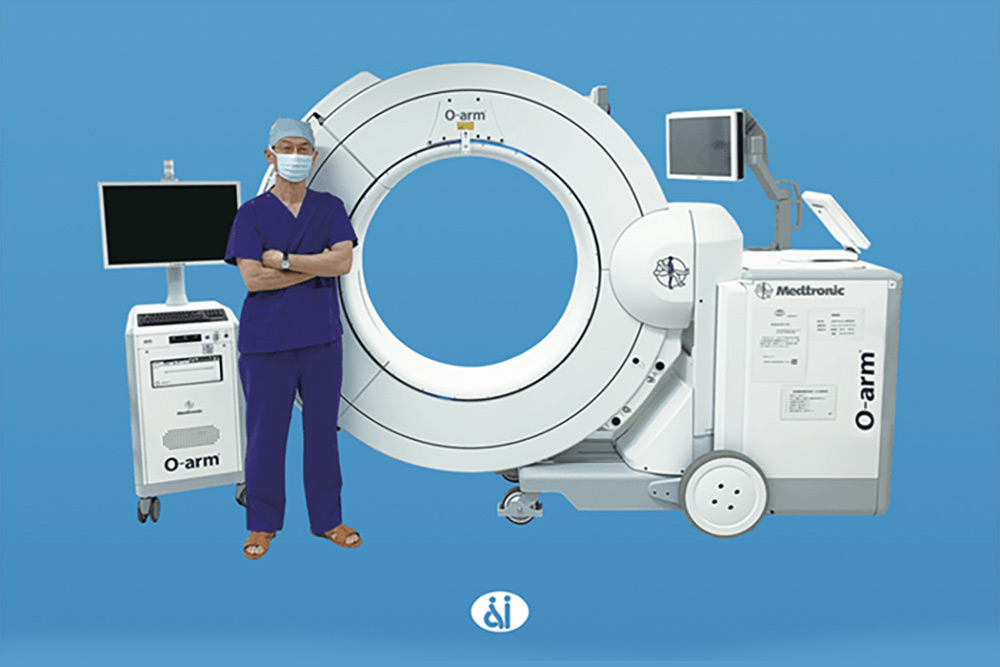
Surgery
We have performed more than 700 spinal surgeries every year. Surgeries for acute traumatic patients are performed as quickly as possible. Degenerative disease, spinal tumour, and spinal deformities are also targeted. The navigation system (O-arm; Medtronic, USA) has been introduced to make complicated surgeries as safe and secure as possible by inserting screws and accurately understanding the orientation of the operating field. This device makes it easier to challenge more difficult surgeries.
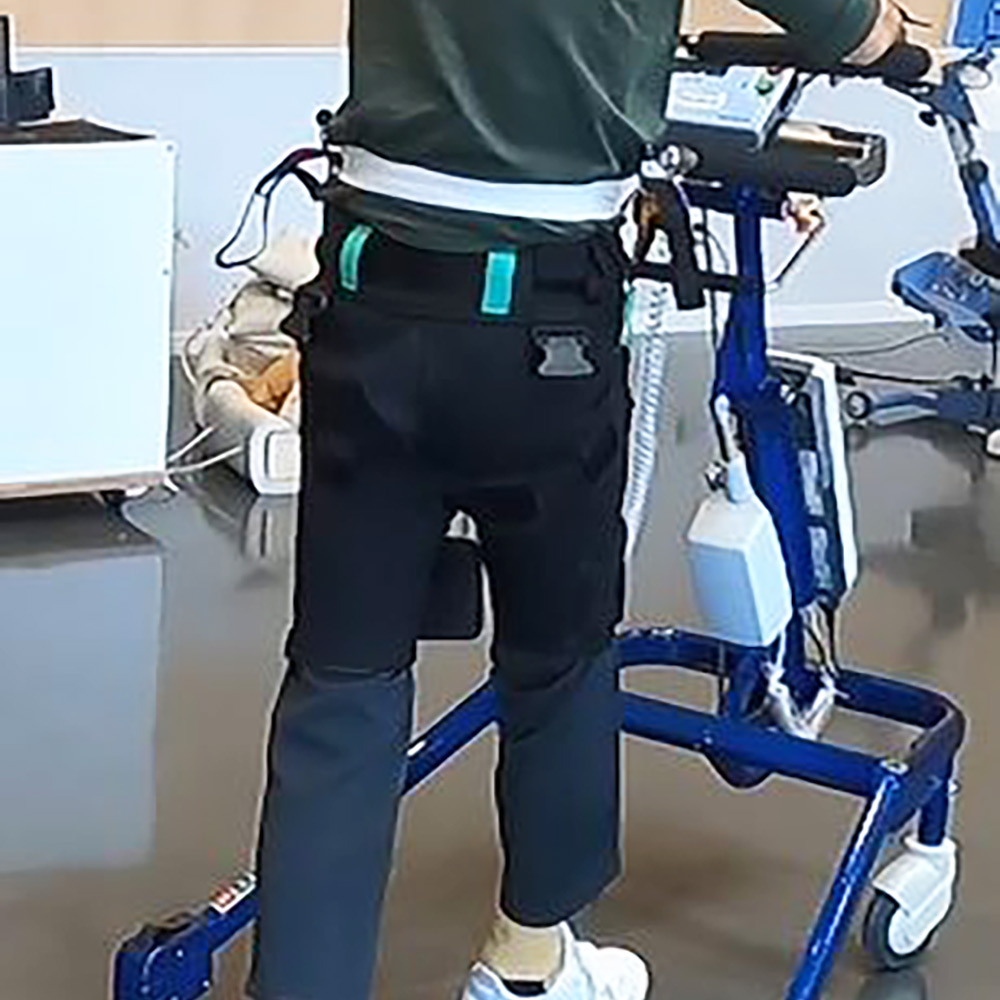
Rehabilitation
Bedside rehabilitation starts from the early phase of spinal cord injury. The rehabilitation of severely paralysed individuals is special and unique because the lifestyle of patients dramatically changes. Special rehabilitation devices such as therapeutic electric stimulation and walk assist robots have been utilised, facilitating patient neurological and functional recovery. We also maintain a comprehensive database of patient information regarding the clinical time course of neurological status, ADL, physical ability, etc.
Collaboration among all the departments
Discussion among all departments about the patients’ problems is important because the condition of patients with paralysis dramatically changes after injury. Collaboration among medical doctors, nurses, therapists, architects, and social workers plays an important role in coping with the patients’ problems. We regularly discuss rehabilitation goals, timing of discharge, mental problems, social resources, and necessity of house renovation.
What is special?
The Spinal Injuries Centre is located at Iizuka City in Fukuoka Prefecture on a hill surrounded by trees along the National Road, Route 201, and enjoys an environment most suitable for medical facilities for individuals with serious disabilities.
Address: 550-4, Igisu, Iizuka City, Fukuoka Prefecture, 820-8508, JAPAN
Guide to the Centre
Access
Use of the JR Fukuhoku-Yutaka Line from Hakata Station (Fukuoka City) or Kurosaki Station (Kitakyushu City)
Disembark at “Shin-Iizuka” Station
Taxi: 15 minutes by taxi from “Shin-Iizuka” Station
Nishitetsu Bus
Shin-Iizuka Station→(10 min)→Iizuka Bus Centre→(20 minutes)→Spinal Injuries Centre or Higashi-Ikawa
Historical Background
In 1974, the Labor Ministry recognised that the current situation of spinal cord injury patients staying in the existing facilities for a long period of time resulted in the lagging of their social comeback compared the developed countries such as the United States and Europe, and launched a plan to establish advanced and specialised medical facilities for spinal cord injury and other patients as one of the Labor Ministry’s important policies for the fiscal year 1975.
The Labor Welfare Corporation (currently known as the Japan Organization of Occupational Health and Safety), in co-operation with the Employment Promotion Corporation, extensively studied this plan and investigated the existing status of facilities in Western European countries. This led to an opportune time for the establishment of a spinal injury centre which was planned for construction in Iizuka thanks to the invitation of the Fukuoka Prefecture and Iizuka City governments. Three years after the land development work was inaugurated in November 1976, the construction of the Centre was finally completed in March 1979 and opened to the public on June 1, 1979.
We welcome foreign doctors to the opportunity to study abroad
We have accepted many foreign doctors who need to learn how to comprehensively treat spinal cord injuries, including surgery, rehabilitation, nursing, return to work, and housing renovation. We have had many foreign doctors visit our centre to learn. From 2010 to 2020, we accepted 16 excellent doctors who were willing to study abroad (nine from Thailand, three from Vietnam, two from Afghanistan, one from France, and one from El Salvador). We can offer a cosy dormitory and a small amount of financial livelihood support. We welcome motivated foreign doctors who want to study abroad to learn how to perform a comprehensive treatment for patients with spinal cord injuries.

Medical Doctors
- Takeshi Maeda Deputy president
- Osamu Kawano Vice president
Department of Orthopedic Surgery
- Hiroaki Sakai Director
- Muneaki Masuda
- Yuichiro Morishita
- Tetsuo Hayashi
- Kensuke Kubota Vice Director
- Kazu Kobayakawa
- Kazuya Yokota
- Hironari Kaneyama Medical Staff
Department of Rehabilitation Medicine
- Tetsuo Hayashi Director
- Kensuke Kubota Vice Director
- Hironari Kaneyama Medical Staff
Department of Urology
- Ryosuke Takahashi Director
- Kenjiro Imada Medical staff
Recent Publications
- Kawano O, Maeda T, Mori E, Takao T, Sakai H, Masuda M, Morishita Y, Hayashi T,
Kubota K, Kobayakawa K, Kaneyama H.
How much time is necessary to confirm the diagnosis of permanent complete cervical spinal cord injury?
Spinal Cord. 2020 Mar;58(3):284-289. - Hayashi T, Fujiwara Y, Sakai H, Kubota K, Kawano O, Mori E, Takao T, Masuda M,
Morishita Y, Maeda T.
The time course of dysphagia following traumatic cervical spinal cord injury: a prospective cohort study.
Spinal Cord. 2020 Jan;58(1):53-57. - Yokota K, Maeda T, Kawano O, Mori E, Takao T, Sakai H, Masuda M, Morishita Y, Hayashi T, Kubota K, Nakashima Y.
Progression of local kyphosis after conservative treatment for compressive cervical spine fracture with spinal cord injury.
J Orthop Surg Res. 2019 Apr 11;14(1):98. - Koga R, Sasaki T, Ideta R, Iwahashi K, Tsugami C, Nishimura A, Hayashi T, Sakai H, Maeda T.
The EQ-5D-5L in patients admitted to a hospital in Japan with recent spinal cord injury: a descriptive study.
Spinal Cord. 2019 Nov;57(11):960-965. - Kawano O, Masuda M, Takao T, Sakai H, Morishita Y, Hayashi T, Ueta T, Maeda T.
The dosage and administration of long-term intrathecal baclofen therapy for severe spasticity of spinal origin. Spinal Cord. 2018 Oct;56(10):996-999. - Mori E, Ueta T, Maeda T, Ideta R, Yugue I, Kawano O, Shiba K.
Sequential neurological improvements after conservative treatment in patients with complete motor paralysis caused by cervical spinal cord injury without bone and disc injury.
J Neurosurg Spine. 2018 Jul;29(1):1-9. - Yugue I, Okada S, Maeda T, Ueta T, Shiba K. Sensitivity and specificity of the 'knee-up test' for estimation of the American Spinal Injury Association Impairment Scale in patients with acute motor incomplete cervical spinal cord injury.
Spinal Cord. 2018 Apr;56(4):347-354. - Iwahashi K, Hayashi T, Watanabe R, Nishimura A, Ueta T, Maeda T, Shiba K.
Effects of orthotic therapeutic electrical stimulation in the treatment of patients with paresis associated with acute cervical spinal cord injury: a randomized control trial.
Spinal Cord. 2017 Dec;55(12):1066-1070. - Kawano O, Maeda T, Mori E, Yugue I, Ueta T, Shiba K. A Safe Surgical Procedure
for Old Distractive Flexion Injuries of the Subaxial Cervical Spine. Asian Spine
J. 2017 Dec;11(6):935-942. - Matsushita A, Maeda T, Mori E, Yuge I, Kawano O, Ueta T, Shiba K. Can the acute magnetic resonance imaging features reflect neurologic prognosis in patients with cervical spinal cord injury? Spine J. 2017 Sep;17(9):1319-1324.
- Morishita Y, Masuda M, Maeda T, Ueta T, Shiba K. Morphologic Evaluation of Lumbosacral Nerve Roots in the Vertebral Foramen: Measurement of Local Pressure
of the Intervertebral Foramen.
Clin Spine Surg. 2017 Jul;30(6):E839-E844. - Yugue I, Okada S, Masuda M, Ueta T, Maeda T, Shiba K. "Knee-up test" for easy
detection of postoperative motor deficits following spinal surgery.
Spine J. 2016 Dec;16(12):1437-1444. - Takao T, Okada S, Morishita Y, Maeda T, Kubota K, Ideta R, Mori E, Yugue I, Kawano O, Sakai H, Ueta T, Shiba K. Clinical Influence of Cervical Spinal Canal Stenosis on Neurological Outcome after Traumatic Cervical Spinal Cord Injury without Major Fracture or Dislocation.
Asian Spine J. 2016 Jun;10(3):536-42. - Hayashi T, Maeda T, Masuda M, Ueta T, Shiba K. Morphology of the injured posterior wall causing spinal canal encroachment in osteoporotic vertebral fractures.
Spine J. 2016 Aug;16(8):946-50. - Masuda M, Ueta T, Shiba K, Iwamoto Y.
D-dimer screening for deep venous thrombosis in traumatic cervical spinal injuries.
Spine J. 2015 Nov 1;15(11):2338-44. - Yugue I, Okada S, Masuda M, Ueta T, Maeda T, Shiba K.
Risk factors for adjacent segment pathology requiring additional surgery after single-level spinal fusion: impact of pre-existing spinal stenosis demonstrated by preoperative
myelography.
Eur Spine J. 2016 May;25(5):1542-1549. - Vu TT, Morishita Y, Yugue I, Hayashi T, Maeda T, Shiba K. Radiological Outcome of Short Segment Posterior Instrumentation and Fusion for Thoracolumbar Burst Fractures.
Asian Spine J. 2015 Jun;9(3):427-32. - Mori E, Ueta T, Maeda T, Yugue I, Kawano O, Shiba K.
Effect of preservation of the C-6 spinous process and its paraspinal muscular attachment on the prevention of postoperative axial neck pain in C3-6 laminoplasty.
J Neurosurg Spine. 2015 Mar;22(3):221-9. - Kobayakawa K, Kumamaru H, Saiwai H, Kubota K, Ohkawa Y, Kishimoto J, Yokota K, Ideta R, Shiba K, Tozaki-Saitoh H, Inoue K, Iwamoto Y, Okada S.
Acute hyperglycemia impairs functional improvement after spinal cord injury in mice and humans.
Sci Transl Med. 2014 Oct 1;6(256):256ra137. - Morishita Y, Maeda T, Ueta T, Naito M, Shiba K. Pathophysiological effects of lumbar instrumentation surgery on lumbosacral nerve roots in the vertebral foramen: measurement of local pressure of intervertebral foramen.
Spine (Phila Pa 1976). 2014 Oct 1;39(21):E1256-60. - Kawano O, Maeda T, Mori E, Yugue I, Takao T, Sakai H, Ueta T, Shiba K.
Influence of spinal cord compression and traumatic force on the severity of cervical spinal cord injury associated with ossification of the posterior longitudinal ligament.
Spine (Phila Pa 1976). 2014 Jun 15;39(14):1108-12. - Morishita Y, Maeda T, Ueta T, Naito M, Shiba K.
Dynamic somatosensory evoked potentials to determine electrophysiological effects on the spinal cord during cervical spine extension: clinical article.
J Neurosurg Spine. 2013 Sep;19(3):288-92. - Takao T, Morishita Y, Okada S, Maeda T, Katoh F, Ueta T, Mori E, Yugue I, Kawano O, Shiba K.
Clinical relationship between cervical spinal canal stenosis and traumatic cervical spinal cord injury without major fracture or dislocation.
Eur Spine J. 2013 Oct;22(10):2228-31. - Hayashi T, Kawano O, Sakai H, Ideta R, Ueta T, Maeda T, Mori E, Yugue I, Takao T, Masuda M, Morishita Y, Shiba K. The potential for functional recovery of upper extremity function following cervical spinal cord injury without major bone injury.
Spinal Cord. 2013 Nov;51(11):819-22. - Hayashi T, Ueta T, Kubo M, Maeda T, Shiba K. Subarachnoid-subarachnoid bypass: a new surgical technique for posttraumatic syringomyelia.
J Neurosurg Spine. 2013 Apr;18(4):382-7. - Yugue I, Okada S, Ueta T, Maeda T, Mori E, Kawano O, Takao T, Sakai H, Masuda M, Hayashi T, Morishita Y, Shiba K.
Analysis of the risk factors for tracheostomy in traumatic cervical spinal cord injury. Spine (Phila Pa 1976). 2012 Dec 15;37(26):E1633-8. - Maeda T, Ueta T, Mori E, Yugue I, Kawano O, Takao T, Sakai H, Okada S, Shiba K.
Soft-tissue damage and segmental instability in adult patients with cervical spinal cord injury without major bone injury. Spine (Phila Pa 1976). 2012 Dec 1;37(25):E1560-6. - Hayashi T, Maeda T, Ueta T, Shiba K, Iwamoto Y. Comparison of the amounts of canal encroachment between semisitting and supine position of computed tomography-myelography for vertebral fractures of the elderly involving the posterior vertebral wall.
Spine (Phila Pa 1976). 2012 Sep 1;37(19):E1203-8. - Mori E, Okada S, Ueta T, Itaru Y, Maeda T, Kawano O, Shiba K.
Spinous process-splitting open pedicle screw fusion provides favorable results in patients with low back discomfort and pain compared to conventional open pedicle screw fixation over 1 year after surgery. Eur Spine J. 2012 Apr;21(4):745-53. - Yugue I, Aono K, Shiba K, Ueta T, Maeda T, Mori E, Kawano O.
Analysis of the risk factors for severity of neurologic status in 216 patients with thoracolumbar and lumbar burst fractures.
Spine (Phila Pa 1976). 2011 Sep 1;36(19):1563-9.